SPIOLTO® Respimat® (tiotropium + olodaterol) for COPD
SPIOLTO Respimat
SPIOLTO Respimat
SPIOLTO Respimat (tiotropium + olodaterol) is indicated as a maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD).1

Mechanism of Action
SPIOLTO Respimat is a fixed dose combination inhalation solution containing the long-acting muscarinic receptor antagonist (LAMA) tiotropium, and the long-acting beta agonist (LABA) olodaterol, which is delivered via the Respimat soft mist inhaler device. The two active ingredients provide additive bronchodilation due to their different modes of action. Since muscarinic receptors appear to be more prominent in the central airways while beta2-adrenoceptors have a higher expression level in the peripheral airways, a combination of tiotropium and olodaterol should provide optimal bronchodilatation in all regions of the lungs.1
Tiotropium — tiotropium bromide is a long-acting, specific antagonist at muscarinic receptors.1
Olodaterol — olodaterol has a high affinity and high selectivity to the human beta2-adrenoceptor.1
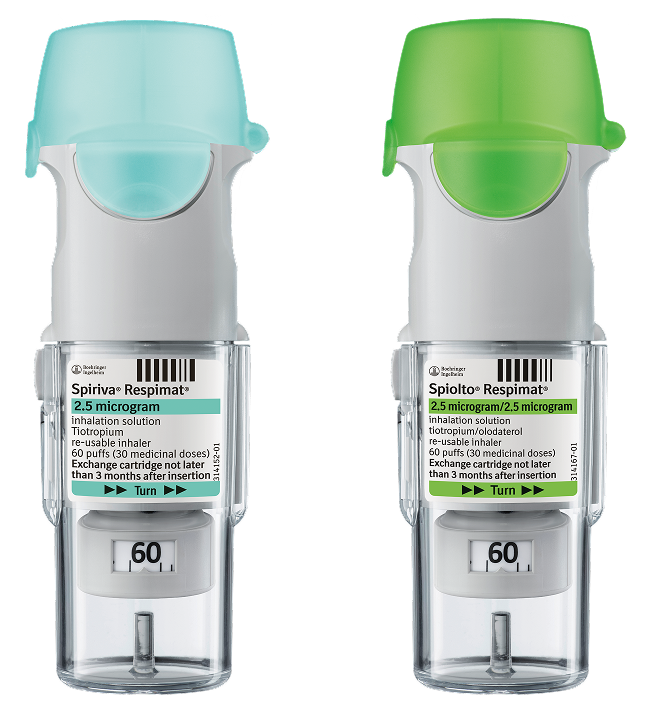
The benefit of switching to SPIOLTO Respimat (tiotropium + olodaterol): from SPIRIVA® Respimat
TONADO: Two replicate, randomised, double-blind, active-controlled, phase III trials comparing SPIOLTO Respimat with SPIRIVA Respimat (tiotropium) and olodaterol Respimat over 52 weeks in 5,162 adult patients with moderate to very severe COPD. The primary endpoints were lung function measured as FEV1 AUC0–3h and trough FEV1 response in each individual trial, and SGRQ total score (combined analysis of both trials) at 24 weeks.2
OTEMTO: Two replicate, randomised, double-blind, placebo-controlled, phase IIIb trials comparing SPIOLTO Respimat with SPIRIVA Respimat (tiotropium) and placebo Respimat over 12 weeks in 1,621 adult patients with moderate to severe COPD. The primary endpoints were SGRQ total score, and lung function measured as FEV1 AUC0–3h and trough FEV1 response in each individual trial.3
If COPD is not controlled while using a LAMA monotherapy — such as SPIRIVA Respimat (tiotropium) — escalation to a dual LAMA + LABA therapy — like SPIOLTO Respimat — could offer symptom control in important priority areas while maintaining inhaler continuity.*2-4
*Priority areas in COPD management include lung function, breathlessness and overall health status 2,4

| SPIOLTO Respimat significantly improved lung function vs SPIRIVA Respimat2,3,5,6The TONADO studies showed SPIOLTO Respimat significantly improved mean FEV1 AUC0–3h (difference of 110mL; p<0.0001) and trough FEV1 (difference of 60mL; p<0.0001) vs SPIRIVA Respimat.2,5 The OTEMTO studies showed SPIOLTO Respimat significantly improved mean FEV1 AUC0–3h (difference of 108mL; p<0.0001) and trough FEV1 (difference of 37mL; p<0.01) vs SPIRIVA Respimat.3,6 |

| SPIOLTO Respimat significantly improved breathlessness vs SPIRIVA Respimat2,3TONADO showed a mean TDI focal score of 1.98 units for SPIOLTO Respimat, with a significant improvement compared to SPIRIVA Respimat (mean difference 0.36, p<0.05).2 The OTEMTO studies showed a mean improvement in TDI focal score of 0.59 units (p<0.01) with SPIOLTO Respimat vs SPIRIVA Respimat.3 |

| SPIOLTO Respimat's health-related QoL vs SPIRIVA Respimat1,2TONADO trial showed the proportion of patients with a clinically meaningful decrease in SGRQ total score was greater for SPIOLTO Respimat (57.5%) vs SPIRIVA Respimat (48.7%) (p=0.0001).2 OTEMTO showed the proportion of patients with a clinically meaningful decrease in SGRQ total score was greater for SPIOLTO Respimat (52%) vs SPIRIVA Respimat (41%) (p=0.0022).1 |

| Maintaining inhaler continuityGOLD strategy recommends that if a patient is taking an inhaled therapy and able to use their device correctly, any new therapy is best prescribed in the same device. For patients currently prescribed SPIRIVA Respimat who are advised to switch to a LAMA + LABA, moving to SPIOLTO Respimat enables them to keep the inhaler they are familiar with.4 |
Once-daily SPIOLTO Respimat is generally well-tolerated2
TONADO: two replicate, randomised, double-blind, parallel-group, active-controlled, phase III trials comparing SPIOLTO Respimat with SPIRIVA Respimat (tiotropium) and olodaterol Respimat over 52 weeks in 5,162 adult patients with moderate to very severe COPD. The primary endpoints were lung function measured as FEV1 AUC0–3h and trough FEV1 response in each individual trial, and SGRQ total score (combined analysis of both trials) at 24 weeks.2
SPIOLTO Respimat was generally well-tolerated with an adverse event profile similar to the profiles of the monotherapies (tiotropium and olodaterol).1,2,7,8
Most adverse events were mild or moderate with no new safety risks seen beyond the known effects of the ingredients.1,2,7,8
The proportion of patients who discontinued SPIOLTO Respimat due to an adverse event was comparable to SPIRIVA Respimat or olodaterol Respimat.
Tabulated summary of adverse events
The frequencies assigned to the undesirable effects listed below are based on the crude incidence rates of adverse drug reactions (i.e. events attributed to SPIOLTO Respimat) observed in the tiotropium 5 microgram/olodaterol 5 microgram dose group (5646 patients), pooled from 8 active or placebo-controlled, parallel group clinical trials in COPD patients with treatment periods ranging between 4 and 52 weeks.1
Adverse reactions reported in all clinical trials with SPIOLTO Respimat are shown below according to system organ class. These also include all adverse reactions previously reported with one of the individual components.1
Frequency is defined using the following convention:1 Very common (≥ 1/10); common (≥ 1/100 to <1/10); uncommon (≥ 1/1,000 to <1/100); rare (≥ 1/10,000 to <1/1,000); very rare (<1/10,000), not known (cannot be estimated from the available data)
| System Organ Class | Adverse reaction | Frequency |
| Infections and infestations | Nasopharyngitis | Not known |
| Metabolism and nutrition disorders | Dehydration | Not known |
| Nervous system disorders | Dizziness | Uncommon |
| Insomnia | Rare | |
| Headache | Uncommon | |
| Eye disorders | Vision blurred | Rare |
| Glaucoma | Not known | |
| Intraocular pressure increased | Not known | |
| Cardiac disorders | Atrial fibrillation | Rare |
| Tachycardia | Uncommon | |
| Palpitations | Rare | |
| Supraventricular tachycardia | Rare | |
| Vascular disorders | Hypertension | Rare |
| Respiratory, thoracic and mediastinal disorders | Cough | Uncommon |
| Dysphonia | Uncommon | |
| Laryngitis | Rare | |
| Pharyngitis | Rare | |
| Epistaxis | Rare | |
| Bronchospasm | Rare | |
| Sinusitis | Not known | |
| Gastrointestinal disorders | Dry mouth | Uncommon |
| Constipation | Rare | |
| Oropharyngeal candidiasis | Rare | |
| Gingivitis | Rare | |
| Nausea | Rare | |
| Intestinal obstruction Ileus paralytic | Not known | |
| Dysphagia | Not known | |
| Gastrooesophageal reflux disease | Not known | |
| Glossitis | Not known | |
| Stomatitis | Rare | |
| Dental caries | Not known | |
| Skin and subcutaneous tissue disorders, Immune system disorders | Hypersensitivity | Rare |
| Angioedema | Rare | |
| Urticaria | Rare | |
| Pruritus | Rare | |
| Anaphylactic reaction | Not known | |
| Rash | Rare | |
| Skin infection and skin ulcer | Not known | |
| Dry skin | Not known | |
| Musculoskeletal and connective tissue disorders | Arthralgia | Rare |
| Back pain1 | Rare | |
| Joint swelling | Rare | |
| Renal and urinary disorders | Urinary retention | Rare |
| Urinary tract infection | Rare | |
| Dysuria | Rare |
Serious undesirable effects consistent with anticholinergic effects: glaucoma, constipation, intestinal obstruction including ileus paralytic and urinary retention. An increase in anticholinergic effect may occur with increasing age.
Undesirable effects related to the beta-adrenergic agonist class, which are not listed above, should be taken into consideration. These include arrhythmia, myocardial ischaemia, angina pectoris, hypotension, tremor, nervousness, muscle spasms, fatigue, malaise, hypokalemia, hyperglycemia, and metabolic acidosis.
Please refer to the Summary of Product Characteristics for a complete list of adverse events.
The benefit of switching to SPIOLTO Respimat (tiotropium + olodaterol): from a DPI
Advantages of the Respimat Soft Mist Inhaler
Not all patients with COPD have the ability to generate enough inspiratory flow to inhale their medication correctly.9
Various inhaler characteristics will influence a patients' inhaler preference, including ease of use, convenience, and environmental impact. The ideal inhaler will also deliver the drug dose to the lungs, regardless of inspiratory flow.10
The Respimat Soft Mist Inhaler provides a consistent dose to the lungs, independent of inspiratory ability.†,11,12

| Ability to inhale | Respimat: lower inspiratory effort expected compared to tested DPIs†‡11,12 Respimat requires a lower inspiratory effort to achieve optimal flow rate compared with tested DPIs. |

| Drug lung deposition | Respimat: greater drug lung deposition vs tested DPIs†‡,11,12 |

| Inhaler technique | Respimat: "slow and steady" inhalation13Respimat requires "slow and steady" inhalation, compared with the "quick and deep" inhalation required by DPIs. |
Footnotes
†Lower inspiratory effort expected to achieve optimal flow rate from an in vitro study, where air flow resistance was compared between different devices at specified flow rates.12 Recommended inspiratory flow rates are specific to each device.
‡These studies simulated the upper airways (in vitro) and the lower airways (in silico) of patients with moderate and very severe COPD. For very severe COPD breathing patterns, the modelled dose delivered to lungs was 67% of the nominal dose with Respimat (tiotropium) vs 51% with Breezhaler® (glycopyrronium), 42% with Genuair® (aclidinium), 55% with Ellipta® (vilanterol), and 41% with Ellipta® (fluticasone). Vilanterol and fluticasone were measured separately when delivered from a nominal dose, delivered as combination of vilanterol and fluticasone from the Ellipta® device.12 For the Respimat (tiotropium + olodaterol) fixed-dose combination, the nominal dose delivered to the lung was 69% (tiotropium) and 72% (olodaterol).11 Vilanterol and fluticasone are not licensed as monotherapy agents through the Ellipta® device.
Abbreviations
AUC0–3h, area under the curve 0–3 hours; COPD, chronic obstructive pulmonary disease; DPI, dry powder inhaler; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; LABA, long-acting beta-agonist; LAMA, long-acting muscarinic antagonist; MCID, minimal clinically important difference; QoL, Quality of Life; SGRQ, St George’s Respiratory Questionnaire; SMI, soft mist inhaler; TDI, Transitional Dyspnoea Index.
Breezhaler® is a registered trademark of Novartis, Genuair® is a registered trademark of AstraZeneca, Ellipta® is a registered trademark of GlaxoSmithKline.
SPIRIVA Respimat (tiotropium) is indicated as a maintenance bronchodilator treatment to relieve symptoms of adult patients with chronic obstructive pulmonary disease (COPD).
SPIOLTO Respimat (tiotropium + olodaterol) is indicated as a maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD).
References
- SPIOLTO® Respimat (tiotropium + olodaterol) Summary of Product Characteristics
- Buhl R, et al. Eur Respir J. 2015;45:969‒979 and supplementary material.
- Singh D, et al. Respir Med. 2015;109(10):1312–9 and supplementary material.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: 2025 Report. Available at: https://goldcopd.org/2024-gold-report/ (Accessed March 2025).
- Boehringer Ingelheim Data on File TOL 14-05(b).
- Singh D, et al. European Respiratory Society International Congress, Amsterdam, The Netherlands, 26–30 September 2015; PA2958.
- SPIRIVA® Respimat (tiotropium) Summary of Product Characteristics.
- STRIVERDI® Respimat (olodaterol) Summary of Product Characteristics
- Mahler DA. Ann Am Thorac Soc. 2017;14:1103–7.
- Dekhuijzen PNR, et al. Patient Prefer Adherence. 2016;10:1561–72.
- Ciciliani AM, et al. Ann Am Thorac Soc COPD. 2021;18(1):91−100.
- Ciciliani AM, et al. Int J Chron Obstruct Pulmon Dis. 2017;12:1565–77.
- Murphy A. How to help patients optimise their inhaler technique. Pharm J. 2016;297(7891)
PC-GB-109565 V1 March 2025