SPIRIVA® Respimat® significantly delayed the time to first severe asthma exacerbation* by 56 days vs placebo Respimat in adults with severe asthma.1
Time to the first severe asthma exacerbation (pooled data at 48 weeks) was a prespecified co-primary endpoint.
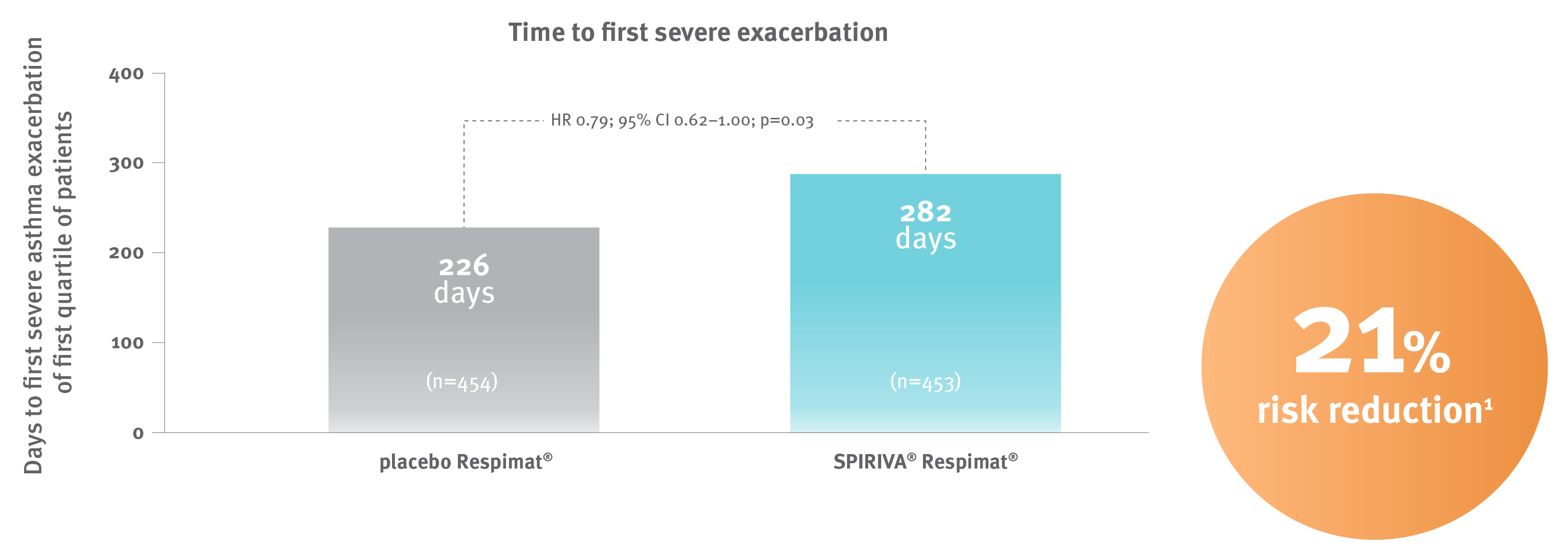
In the tiotropium group, 122 of 453 patients (26.9%) had at least 1 severe exacerbation, as compared with 149 of 454 (32.8%) in the placebo group.1
* Severe asthma exacerbation was defined as a deterioration of asthma necessitating initiation or at least a doubling of systemic glucocorticoids for ≥3 days.1
Adapted from Kerstjens HA et al. 2012.1
PrimoTinA Study Design
Two replicate randomised controlled trials (PrimoTinA-Asthma 1 and PrimoTinA-Asthma 2) compared SPIRIVA Respimat with placebo Respimat over 48 weeks as add-on controller therapy on top of usual care in adult patients with severe asthma who were symptomatic on maintenance treatment of at least ICS (≥800 μg budesonide/day or equivalent) plus LABA, had a post-bronchodilator FEV1 of ≤80% of the predicted value and a history of ≥1 severe exacerbation in the previous year. In both the SPIRIVA Respimat and placebo Respimat groups, ICS and LABA maintenance therapy was continued. Other asthma medications were allowed if the doses remained stable for ≥4 weeks before study entry and for the duration of the trial. The co-primary endpoints were lung function measured as peak FEV1(0-3h) and trough FEV1 response at week 24, and time to first severe exacerbation (pooled data) over 48 weeks.1
Abbreviations
ARR, absolute risk reduction; CI, confidence interval; HR, hazard ratio; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist.
Reference: 1. Kerstjens HA et al. N Engl J Med 2012;367:1198–207.